
IMMH Conference
Very pleased to be supporting IMMH at the 11th annual Integrative Medicine for Mental Health Conference, August 20-23, at the historic Hilton Chicago on Michigan Avenue. This four-day international conference will give practitioners a holistic approach to successfully diagnose and treat underlying issues contributing to the symptoms of neurological, behavioral, and psychiatric disorders.
IMMH is the only conference annually dedicated to integrative medicine for mental health, which is brain health.
IMMH will soon be announcing all of the speakers for IMMH 2020. Details, including registration available at www.IMMH2020.com. Stay tuned for updates.
In the meantime, check out the highlight video from this year’s IMMH Conference:
Sugar in 2020
Happy New Year!
Hopefully, your new year is off to a healthy start.
You may have seen the New York Time article by By :
“Make 2020 the Year of Less Sugar”
and her follow-up piece:
“Dried Fruit, Oats and Coffee: Answers to Your Sugar Questions”
This recent interview with Robin Young (@hereandnowrobin) on Here and Now (@hereandnow/@NPR) references Tara Parker-Pope’s story:
Addicted To Sugar? This Doctor Says It’s ‘The New Tobacco’
I’m in Paris on sabbatical, but if you happen to be in or near San Francisco on January 15th, don’t miss this event at UCSF with my colleagues:
Blood Sugar Health Salon Discussion
1-15-20, 7-8:30pm
Using new tech to prevent chronic #MetabolicDisease rather than just manage it.
Featuring
Dr. Aaron Neinstein @AaronNeinstein (@UCSF)
Dr. Carolyn Jasik / @DrJasik (@omadahealth)
Jessie Inchauspe @jessie_inc_
Hosted by: Hypoglycemia Support Foundation (@Hypoglycemia101) & the UCSF AME Center (@UCSFAME)
Details/RSVP: hypoglycemia.org/salons
All the best to you in this new year.

Sabbatical 2020
Happy New Decade, everyone!
It’s not a secret that children (and really all of society) this past decade have become addicted, depressed, anxious, distracted, and angry.
The question is why. I’m going out on a limb here. We now have two dopamine stimulators that we freely and willingly give to kids — sugar and technology. But the genie is out of the bottle. We have to find a way to peacefully co-exist with these problems, and we have to teach children how to manage them.
For the next six-months, I’m going on sabbatical in Paris, where I will be bridging two academic units — the Center for Research and Interdisciplinarity (https://www.cri-paris.org/en) and the neurocybernetics lab of ETIS (Information Processing and Systems Teams) at the Université de Cergy-Pontoise (https://perso-etis.ensea.fr/
Wish me luck! I’ll need it!

Hyper-Palatable Foods
“betcha can’t eat just one!”
“A popular U.S. brand of potato chips once promoted itself with the slogan, “betcha can’t eat just one!” Maybe that’s because potato chips, like so many foods in the American diet, can pack a mix of ingredients apt to light up people’s brain-reward neural circuitry and overpower mechanisms that are supposed to signal when we’ve had enough to eat. Researchers call this class of foods — often processed foods or sweets with alluring combinations of fat, sugar, carbohydrates and sodium — “hyper-palatable.” While a slew of films, popular books and academic studies have addressed hyper-palatable foods over the past 15 or so years, none has yet to offer a broadly accepted quantitative definition of just what constitutes a hyper-palatable food.”
New research offers specific metrics that might qualify foods as hyper-palatable — and finds most foods consumed in the United States meet these criteria.
Article: Data-driven definition of unhealthy yet pervasive ‘hyper-palatable’ foods
Research Paper in Obesity: Hyper‐Palatable Foods: Development of a Quantitative Definition and Application to the US Food System Database
“Extensive research has focused on hyper‐palatable foods (HPF); however, HPF are defined using descriptive terms (e.g., fast foods, sweets), which are not standardized and lack specificity. The study purpose was to develop a quantitative definition of HPF and apply the definition to the Food and Nutrient Database for Dietary Studies (FNDDS) to determine HPF prevalence in the US food system.”
“The study is the first to provide a quantitative definition of HPF to be used as a starting point for future research. Given the immense contributions of HPF to obesity risk and related health conditions, it is imperative that the research community develop and validate a specific, quantitative definition of HPF that will advance the field’s understanding of potential mechanisms that may drive overeating and obesity. The HPF definition may also be an asset to inform future food policy work. A major barrier to policy legislation on HPF is that there is no precise definition to inform regulation, and it is not feasible to limit or restrict entire categories of foods (e.g., desserts). Given the ways in which HPF are integrated into our existing food system, strong and specific scientific evidence will be needed to dislodge and eventually regulate some of the most problematic foods that are associated with extensive disease and disability in the US. The HPF definition and quantitative criteria presented in this study represent a crucial first step in this process.”
Article: Study offers data-driven definition of unhealthy yet pervasive ‘hyper-palatable’ foods
“Fazzino and her KU coauthors — Kaitlyn Rohde, research assistant at the Cofrin Logan Center and Debra K. Sullivan of the Department of Dietetics and Nutrition at the University of Kansas Medical Center — sought to define criteria for hyperpalatable foods by conducting a literature review, and then using nutrition software and applying their definition to 7,757 food items in the U.S. Department of Agriculture’s Food and Nutrient Database for Dietary Studies (FNDDS).”
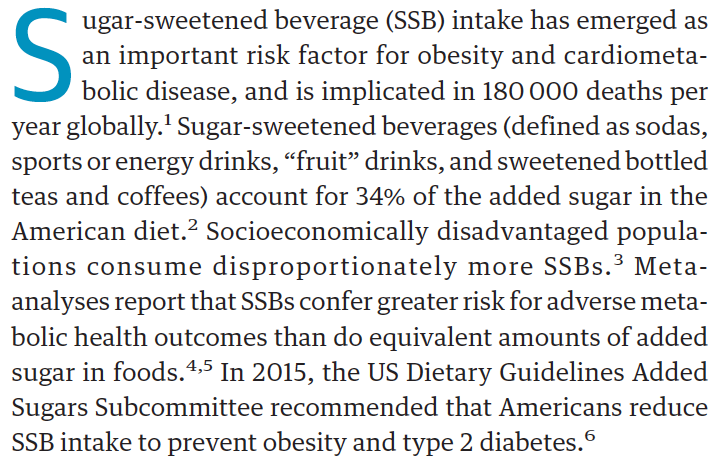
Sales Ban on SSBs Makes an Impact
In this before-after study and trial that included 214 adults who regularly drank SSBs, participants reported consuming less SSBs after a workplace sales ban and a reduction in waist circumference and sagittal diameter but no change in body mass index or insulin sensitivity. Those randomized to receive a brief motivational intervention had greater improvements.
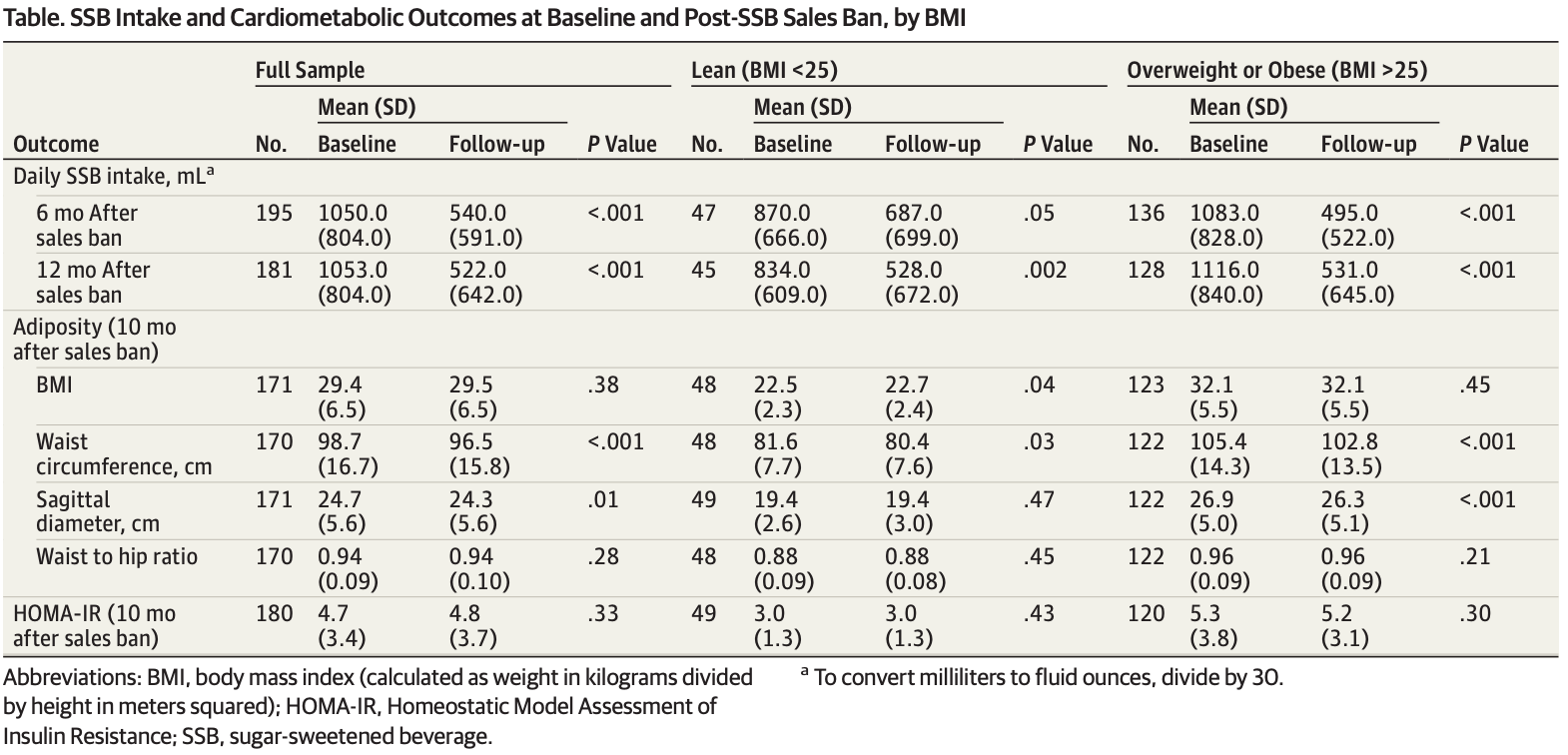
“As rates of cardiometabolic diseases continue to rise, private employers are likely to face greater productivity losses and private health expenditures. The results of this study suggest that workplace SSB sales bans, if widely adopted, could add another layer of efficacy to existing SSB reduction strategies. At the societal level, private sector–driven change through workplace sales bans seems to offer a strategy that complements existing governmental reform efforts. Although effective, governmental reform policies, such as SSB taxation and warning labels, face significant political obstacles that private-sector sales bans do not.”
Articles about the Study
UCSF Banned Sugary Drink Sales, Here Is What Happened Next, Forbes
Sugary Drink Ban Tied to Health Improvements at Medical Center, New York Times
Doctors call on workplaces to ban sale of sugary drinks, The Guardian
Workplace sugary-drink ban helps employees cut back, Reuters
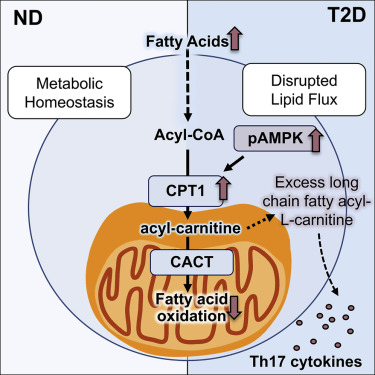
Fat and fructose at the mitochondria that drives the inflammatory process
Paper in Cell Metabolism:
It’s long been known that both “lipotoxicity” and “glucotoxicity” are associated with inflammation leading to diabetes. But it wasn’t clear which, when, and how, resulting in different factions battling for supremacy. The science of this controversy is now beginning to come into focus.
A paper two weeks ago from Softic et al. in Cell Metabolism demonstrates that fructose inhibits mitochondrial beta-oxidation through alteration of specific mitrochondrial proteins, conversely glucose stimulates it. Thus dietary sugar is more metabolically problematic than dietary starch; a finding that our group corroborated in obese children.
This paper from Nicholas et al. also in Cell Metabolism, demonstrates that because of that mitochondrial dysfunction, fatty-acylcarnitine, which should be beta-oxidized, can power the production of TH17 cytokines that in part drive that inflammation. Furthermore, one must remember that some of that fatty acid production can be derived via de novo lipogenesis using fructose as a substrate.
This paper, combined with Softic, helps bridge the gap to show that, at the molecular level, it appears to be the combination of both fat and fructose at the mitochondria that drives the inflammatory process.
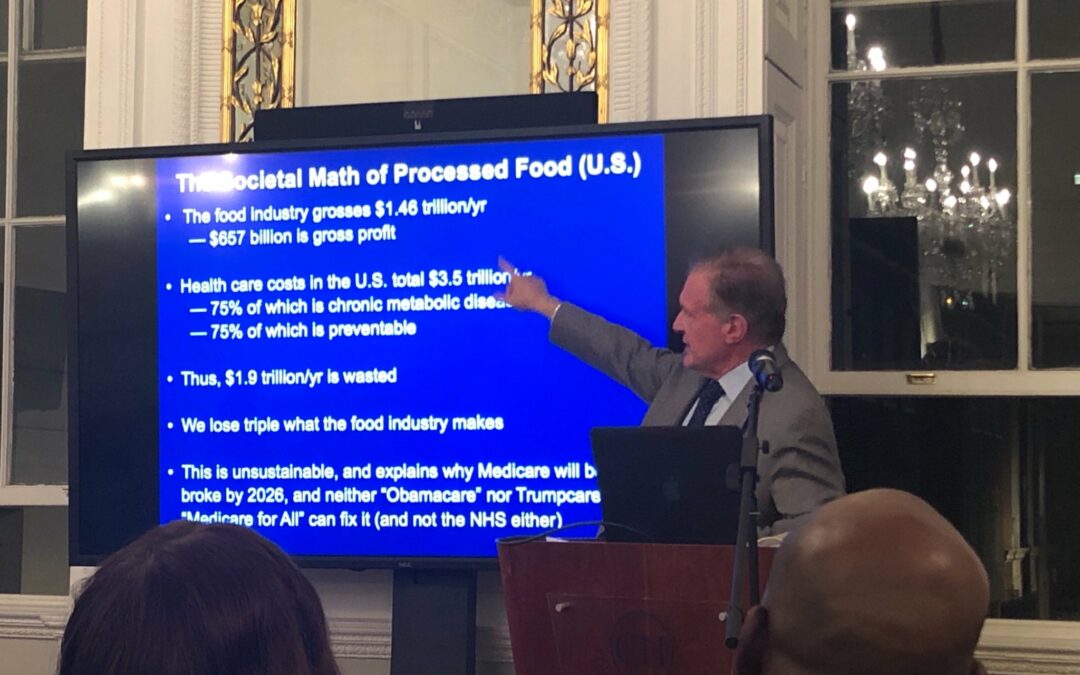
Societal Math
The Societal Math of Processed Food (U.S.)
The food industry grosses 1.46 Trillion / yr
-657 billion is gross profit
Health care costs in the U.S. total $3.5 trillion / yr
-75% of which is chronic metabolic disease
-75% of which is preventable
Thus, $1.9 trillion / yr is wasted.
We lose triple what the food industry makes.
This is unsustainable, and explains why Medicare will be broke by 2026, and neither “Obamacare” or “Trumpcare” or “Medicare for All” can fix it (and not the NHS either).
Fructose Drunk
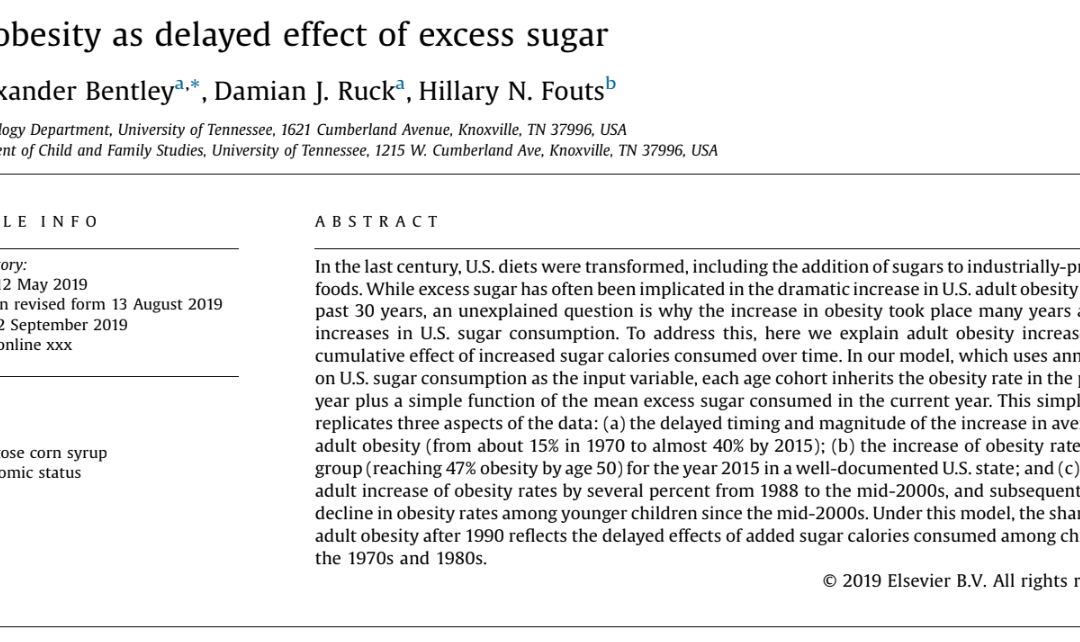
U.S. obesity as delayed effect of excess sugar
This paper is huge. One of the arguments the food industry advances is that sugar consumption has gone down while obesity has gone up, so it can’t be sugar. This paper uses a complex statistical analysis to show that US obesity is a function of both current sugar consumption and an derivative of the sugar consumed by the previous generation going forward. In other words, it’s the economic equivalent of “epigenetics”. This is yet another nail in the coffin (as if we needed any more nails)!
U.S. obesity as delayed effect of excess sugar
https://www.sciencedirect.com/science/article/pii/S1570677X19301364
Synthetic or non-nutritive sweeteners
“The majority of observational studies addressing synthetic or non-nutritive sweeteners (NNS) consumption show an association with metabolic dysregulation.”
Beyond food intake, numerous studies have shown…
animals consuming synthetic sweeteners exhibit weight gain
Feijó et al., 2013
Swithers and Davidson, 2008
Swithers et al., 2010
Swithers et al., 2013
impaired glucose homeostasis
Suez et al., 2014
Swithers et al., 2012
weaker caloric compensation
Swithers et al., 2010
synthetic sweeteners act through the microbiome
Suez et al., 2014
reduced validity of “sweetness” to predict caloric content
Swithers et al., 2010
significant correlation between NNS consumption and weight gain in an 80,000 participants study
Stellman and Garfinkel, 1988
Other independent studies confirmed these associations, with synthetically sweetened beverage consumption being associated with a much higher incidence of metabolic syndrome (odds ratio ∼1.93) when compared to non-users
Fowler et al., 2008
Lutsey et al., 2008
and NNS consumption has been identified as a significant risk factor for metabolic disease
in children
Blum et al., 2005
in middle-aged adults
Dhingra et al., 2007
and in the elderly
Fowler et al., 2015
One study showed that NNS consumers exhibit reduced weight gain
Schulze et al., 2004
however, these participants showed increased risk for developing diabetes in an 8-year follow-up.
Furthermore, human intervention studies have also shown that ingestion of NNS could
enhance appetite
Blundell and Hill, 1986
Rogers and Blundell, 1989
promote hunger
Tordoff and Alleva, 1990
and increase food consumption
Lavin et al., 1997
Rogers and Blundell, 1989
Tordoff and Friedman, 1989a
resulting in impaired glucose tolerance
Pepino et al., 2013
Suez et al., 2014
However, other studies have reported no major effect or weight loss as a result of consuming NNSs
De La Hunty et al., 2006
de Ruyter et al., 2012
Raben et al., 200
The overall impact of NNS on metabolic health remains controversial.
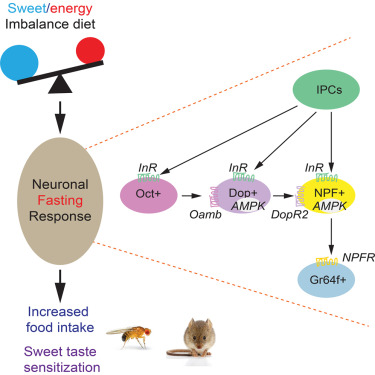
“Despite inclusion in thousands of products, and consumption by billions of people, the molecular effects of ingesting synthetically sweetened food are not well understood. Moreover, there is conflicting evidence from both human and animal studies as to whether or not synthetic sweeteners interact with overall physiology or regulation of energy homeostasis.”
Excerpts from: Sucralose Promotes Food Intake through NPY and a Neuronal Fasting Response
All the studies referenced here are cited and hyperlinked in the article.



